Hashimoto thyroiditis: clinical and diagnostic criteria
Abstract
Hashimoto thyroiditis (HT),
now considered the most common autoimmune disease
, was described over a century ago as a pronounced lymphoid goiter affecting predominantly women.
In addition to this classic form, several other clinico-pathologic entities are now included under the term HT: fibrous variant, IgG4-related variant, juvenile form, Hashitoxicosis, and painless thyroiditis (sporadic or post-partum).
All forms are characterized pathologically by the infiltration of hematopoietic mononuclear cells, mainly lymphocytes, in the interstitium among the thyroid follicles, although specific features can be recognized in each variant.
Thyroid cells undergo atrophy or transform into a bolder type of follicular cell rich in mitochondria called Hürthle cell.
Most HT forms ultimately evolve into
hypothyroidism
, although at presentation patients can be
euthyroid
or even
hyperthyroid
.
The diagnosis of HT relies on the demonstration of circulating antibodies to thyroid antigens (mainly thyroperoxidase and thyroglobulin) and reduced echogenicity on thyroid sonogram in a patient with proper clinical features.
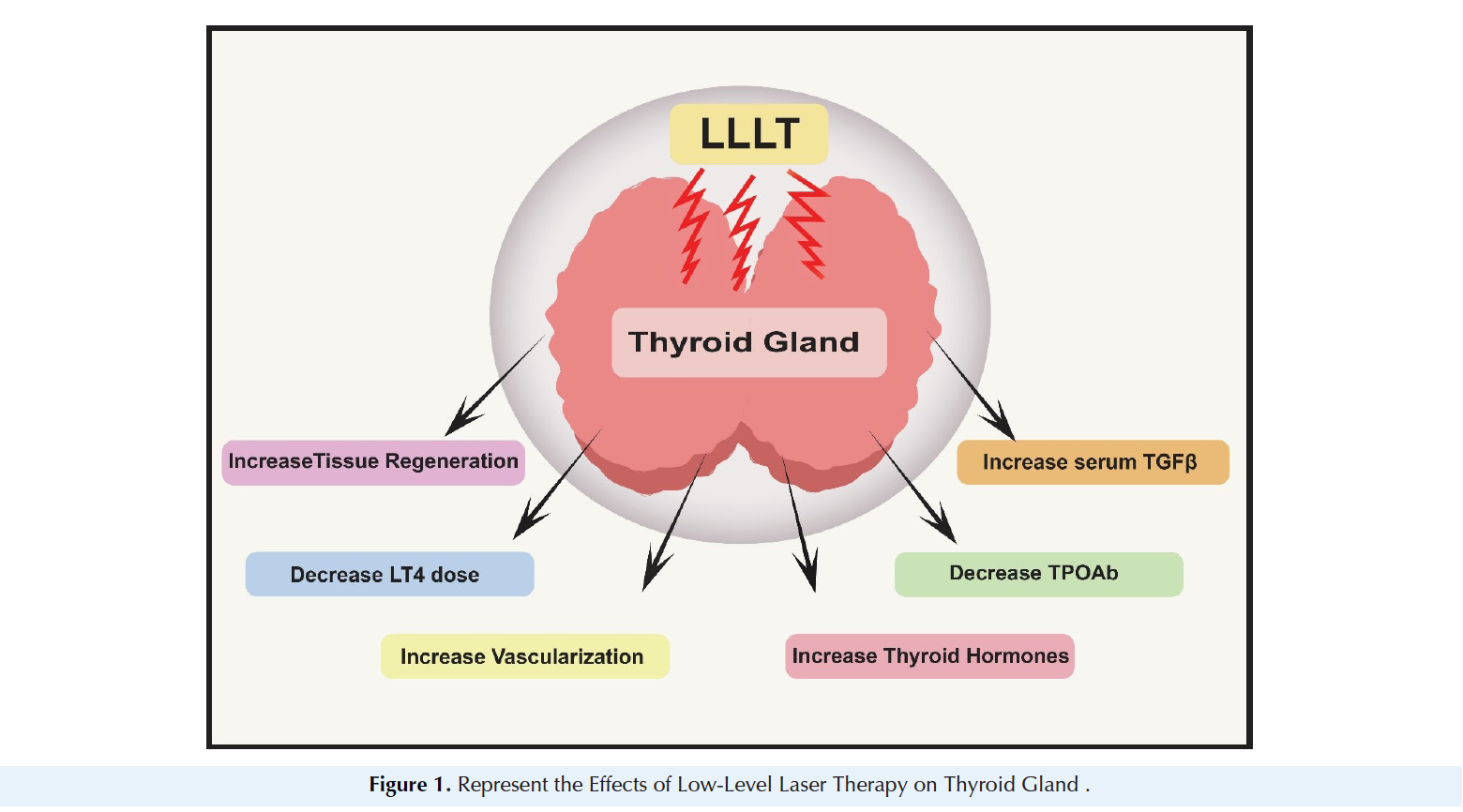
The treatment remains symptomatic and based on the administration of synthetic thyroid hormones to correct the hypothyroidism as needed.
The Knowledge Base on Autoimmune Thyroid is Expanding
This article reflects that our knowledge of autoimmune Hashimoto's thyroid has grown significantly.
What this article reveals, however, is that the standard treatment has not progressed beyond thyroid hormone replacement therapy.
At Johnson Health and Wellness Center, each Hashimoto's patient is given a comprehensive, unique plan designed to specifically meet the individual's needs. We go beyond standard care.
Read More